Why is the Vagus Nerve Important to Physical and Mental Health?
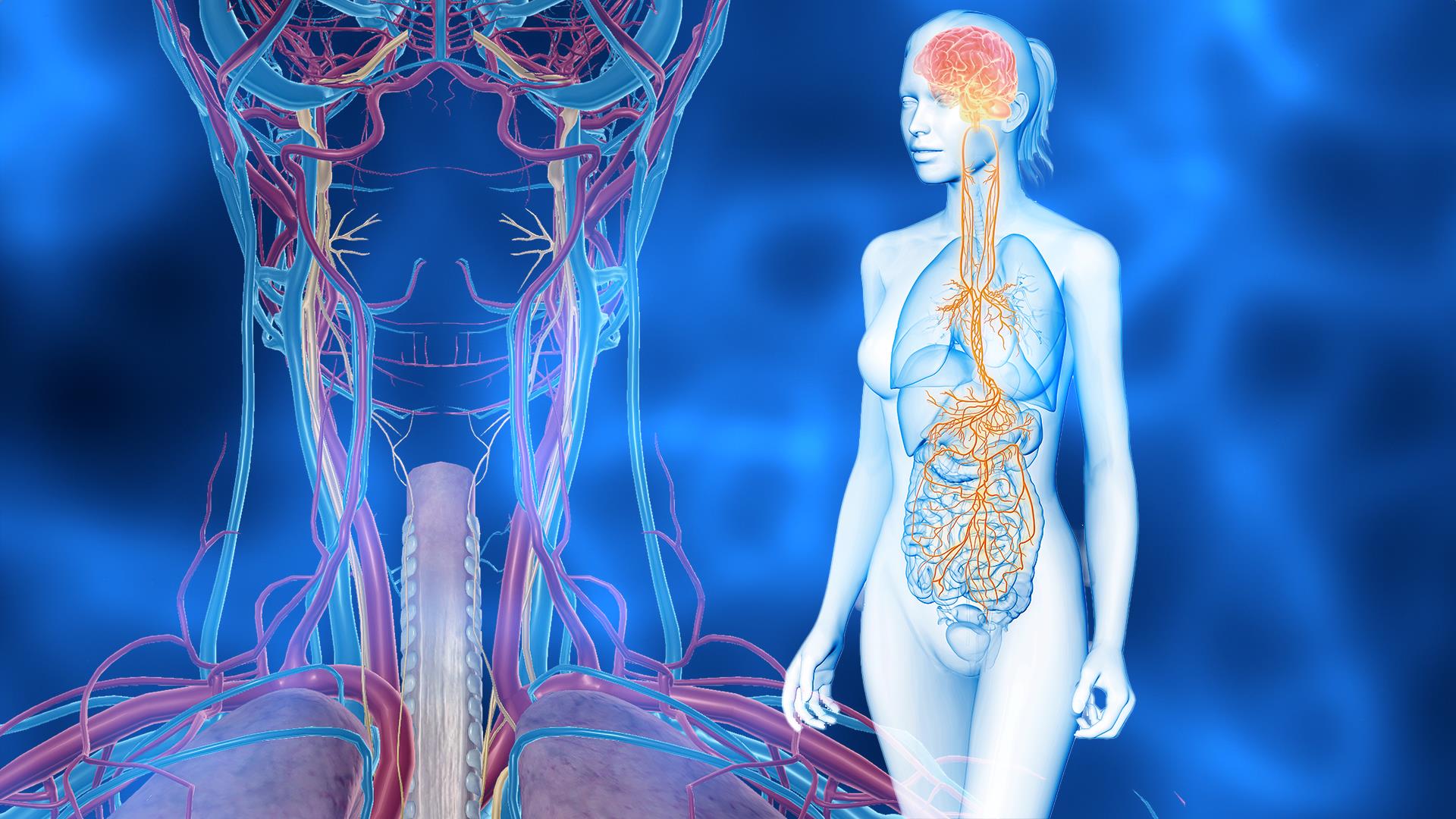
The vagus nerve is the longest cranial nerve, serving as a bidirectional highway between the brainstem and internal organs of the body. This fascinating nerve is significant in modulating homeostasis, integral for regulating various physiological and psychophysiological aspects of health (1).
The vagus, or “wandering nerve,” exerts a profound influence on modulating functions in the body and mind. Composed of two bundles of sensory fibers widely distributed throughout the body, the vagus nerve relays a vast amount of information to the brain regarding its physiological state and functioning. This wandering nerve travels extensively throughout the body, from the brainstem to the neck, chest, heart, lungs, abdomen, and digestive tract. The vagus nerve is constantly receiving, monitoring, and assessing information relative to the conditions of the body and brain. It exerts influence on the autonomic nervous system (ANS), responsible for visceral and involuntary bodily functions such as heart rate, respiration, blood pressure, digestion, and sexual arousal.
Key to the Communication of Multiple Systems
The vagus nerve represents the primary component of the parasympathetic nervous system (PNS), a branch of the autonomic nervous system (ANS) that governs a vast array of important physiological functions, including immune response, mood regulation, digestion, restoration, and heart rate. The sympathetic nervous system is also part of the autonomic system responsible for initiating the body’s “fight, flight, or freeze” mode. The vagus nerve helps to reset this stress response and modulate balance amongst these systems.
The enteric system (ENS) is the third division of the autonomic nervous system, regulating gastrointestinal function with or without input from the central nervous system (CNS). The vagus nerve mediates connection between the ENS and CNS. The ENS, or “second brain,” synthesizes more than 30 neurotransmitters and comprises more than 100 million neurons – far exceeding the amount in the spine (2, 3). Equilibrium amongst these systems is vital for regulating homeostatic functions in the body and is governed by the vagus nerve.
The majority of the communication in the body is termed bottom-up, comprising 80% of the crosstalk that occurs. The vagus nerve fibers are both afferent and efferent, meaning they transmit sensory information from internal organs in the body up to the central nervous system and the brain. The wandering vagus nerve establishes connections between the brain and the gastrointestinal (GI) tract (among other body systems), relaying this information to the brain via these fibers (1).
The vagal afferent and efferent fibers function as part of the PNS, supporting communication among the central, cardiopulmonary, and enteric nervous systems. The vagus nerve communicates tension receptors of the stomach, esophagus, and GI mucosa, as well as any chemical imbalances. Sensory inputs from the liver and pancreas are additionally projected up to the different regions of the brain by the vagus nerve.
HOMEOSTATIC MECHANISMS OF ACTION
Metabolic Regulation Via Vagal Tone – While the pathophysiology of metabolic health conditions (such as obesity, type 2 diabetes, and cardiovascular disease) are multifaceted, we know that it involves communication amongst many organs and systems, including that of the CNS and ENS. The vagus nerve can serve in modulating metabolic mechanisms of health through neuromodulation of these pathways via reductions in neuroinflammation and systemic stress (4). A greater understanding of the interactions between vagal tone, stress, diet, lifestyle, and overall systemic balance and functioning is important since the vagus nerve functions as a bidirectional highway between the body and the brain and thus may be a key, promising targeted approach in improving metabolic health.
Gut-Microbiome & Liver-Brain Axis – The vagus nerve is imperative for modulating the gut-microbiome and gut-liver-brain axis. It serves as the bridge in these pathways with the primary role of regulating systematic, inflammatory, and immune health. The vagus nerve also reduces or inhibits oxidative stress (4).
The liver is essential, as it is responsible for the breakdown of macronutrients and the detoxification of alcohol, medications, and other toxic substances in the body. The liver is also integral for secreting bile. The liver-brain axis mediated by the vagus nerve interacts closely with the central nervous and autonomic nervous systems (5).
The gut-brain-liver axis also influences the control of eating behavior as it receives stimuli from the liver. The neural signs from the central nervous system affect metabolism in the liver. The liver also receives influxes of nutrients and hormones from the GI tract and portal system. Therefore, the GI tract and liver are involved in several imperative immunological interactions mediated by the vagus nerve (4).
Immune Modulation & Stress – The immune modulating effects by the vagus nerve are mediated via the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis comprises the central nervous system and endocrine system and is always adapting to responses of stress or threat (6). The HPA axis is constantly assessing and making modifications as a result of perceived stressors. Emotional stress can induce systemic inflammation that can alter the HPA axis by triggering the release of corticotropin-releasing factor (CRF) from the hypothalamus. CRF then simulates the release of adrenocorticotropic hormone (ACTH) from the pituitary gland. As a result, cortisol is secreted with numerous implications on body systems due to the burden of this stress-induced cascade (7). Improving vagal tone can help in mitigating stress in the system.
Neuromodulatory Effects & The Somatosensory System – Vagal afferent input can stimulate several brain stem nuclei and circuits, thereby affecting various important neurophysiological functions (1). The following brain regions have been found to be implicated during vagal activation: the nucleus tractus solitarius, raphe nucleus, locus coeruleus, thalamus, hypothalamus, amygdala, and cerebral cortex (8). Stimulation of the vagus nerve to these brain regions and structures supports modulation of neurotransmitter concentrations significant for mood, such as norepinephrine and serotonin. These pathways involve autonomic nervous, sensory, and limbic system projections to the neural networks and structures in the brain that govern perception of touch, body temperature, and pain, among other sensations.
Psychophysiology: Mental Health Implications – A growing body of research highlights the connection between inflammation and neural circuits relative to anxiety and depression. Neuromodulation therapies that utilize vagus nerve stimulation may support the reduction of neuroinflammation, thereby improving mood. Therapy modalities shown to attenuate neuroinflammation and reduce proinflammatory factors include Vagus Nerve Stimulation (VNS), Transcranial Magnetic Stimulation (TMS), and Deep Brain Stimulation (DBS) (9, 10). Favorable levels of serotonin, norepinephrine, GABA, and brain-derived neurotrophic factor (BDNF) (key players in the pathophysiology of depression) have been evidenced with use of VNS (11). This further underscores the significance of the vagus nerve and its afferent projections up to the brain.
In addition to modulating the antidepressant response in those with depressive mood disorders, VNS has also been shown to promote neurogenesis in noteworthy brain areas involved in mood, such as the hippocampus (12).
Inflammaging & Vagal Function – The vagus nerve has pronounced anti-inflammatory and anti-aging mechanisms. “Inflammaging” describes the increased burden of worn-out cells, inflammatory cytokines, and dysregulated immune function – all of which contribute to the aging process. Improving vagal tone and function can support many of these processes. Efferent signals transmitted by the vagus nerve via the neurotransmitter acetylcholine pathway can modulate and reduce systemic inflammation. This further highlights the importance of targeting the vagus nerve in order to optimize homeostasis and bodily functions (12).
Vagal Tone, Heart Rate Variability & System Balance – Heart rate is modulated by shifts in the balance of the sympathetic and parasympathetic nervous system. Shifts or variations in heartbeat over time reflect heart rate variability (HRV). HRV provides insight into the tone of the autonomic nervous system. It is also an indicator of stress and how the brain is affected by visceral influences in the body. High coherence or HRV reflects stable, harmonious rhythmic patterns in heartbeat. Correlations between HRV and vagal tone have been well established (13).
The vagus nerve plays a significant role in modulating physiological and psychophysiological homeostasis. Improved vagal tone has not only been associated with greater heart rate variability, but also overall systemic balance and health. Cardiac vagal tone is also a measure of homeostasis, health, and stress in the body.
Vagal afferent fibers from the heart are also distributed to the internal organs of the body, communicating with the nervous and immune systems to modulate regulatory functions via cholinergic and anti-inflammatory pathways (1). These vagal afferents signal activation of the brainstem, resulting in favorable effects on the brain, including those modulated by the HPA axis. The vagus nerve allows bidirectional modifications between the brain and the autonomic nervous systems to influence and modulate hormonal, emotional, metabolic, immune, and neurotransmitter functions (14).
HOW TO STIMULATE VAGAL TONE
HRV – Biofeedback
Vagal tone has been shown to improve with Heart Rate Variability Biofeedback, a treatment in which patients learn self-regulating techniques to utilize in real-time in order to gain insight into the functioning of their physiology, most notably their nervous system (15). Mental health improvements included reductions in stress-related anxiety and depression. Significant improvements in these disorders were most profound when combined with Cognitive Behavioral Therapy (CBT) or other treatments (16).
Breathing & Meditation
Abdominal breathing is a way to manage anxiety as it increases parasympathetic nervous system dominance, as indicated by HRV measurements. Deep and slow breathing, with long exhales, were associated with a significantly reduced state of anxiety in both younger and older adults impacted by physiological stress and anxiety. Deep, slow breathing may be beneficial in restoring vagal outflow and supporting the induced physiological states of anxiety (13).
Vagus Nerve Stimulation (VNS)
As noted, the research relative to Vagus Nerve Stimulation (VNS) is encouraging with far-reaching mind-body health benefits, particularly with regard to psychiatric and GI disorders. VNS treatments that address the vagus nerve, increase or optimize vagal tone, and inhibit cytokine production have been well supported. Stimulation of the vagal afferent fibers in the gut influences the monoaminergic systems of the brain in favorable ways, influencing concentrations of serotonin, dopamine, norepinephrine, and epinephrine (17). In addition to improvements in mood, anxiety disorders, depression, and PTSD, beneficial outcomes have also been demonstrated in gastrointestinal conditions such as IBD (1 ).
Yoga & Acupuncture
Yoga or acupuncture can positively influence vagal tone, providing increased capacity to modulate stress responses. Yoga has been shown to improve vagal tone by helping to establish homeostasis or balance in the system (18). The strategic pressure points of acupuncture are also noteworthy in terms of improving vagal tone and modulating stress (19).
Exercise
Exercise induces positive effects on the body through physiological and biochemical mechanisms via the hypothalamic-pituitary-adrenal HPA axis. It has also been shown to reduce inflammation via vagal tone – which can contribute to better health outcomes for metabolic, immune, and mental health (20).
Lifestyle Factors that Provide Microbiome & Hormonal Support
Addressing the health and diversity of the gut microbiome has been evidenced to have beneficial effects on mood and health, in part by affecting activity of the vagus nerve. In addition to nutrition, lifestyle factors such as stress reduction and adequate sleep further support this. Hormone regulation is also significantly impacted by diet and lifestyle. Ensuring our circadian rhythm is optimally balanced is also integral in supporting systemic balance.
PNI Psychoneuroimmunology
Continued research on the vagus nerve will provide important insights for improving integral aspects of health. The connection between the vagus nerve and immune system regulation is perhaps one of the most exciting developments in this area of research. The vagus nerve has a bidirectional relationship with the immune, enteric system, and that of the central nervous system. The nature of this bidirectional communication is encouraging, with promising implications for addressing the complex interplay between neuroinflammation, autoimmunity, and the manifestation of mental health symptoms.
Improve Vagal Tone to Improve Immunity & Well-Being
Join us on February 27th from 5-7 pm Pacific time for our free online event,Improving Vagus Nervous System Tone: Therapeutic Gateway to the Immune-Nervous Supersystem. Key experts will delve further into this fascinating topic of the vagus nerve and its implications for improved health.
Dr. Jeffrey Bland will discuss the connection between the functioning of the vagus nerve with the immune system then Dr. Peter Staats will dive into pain, inflammation, and the vagus nerve. Navaz Habib will cover clinical approaches to imp
References:
- Fang YT, Lin YT, Tseng WL, Tseng P, Hua GL, Chao YJ, Wu YJ. Neuroimmunomodulation of vagus nerve stimulation and the therapeutic implications. Front Aging Neurosci. 2023 Jul 6;15:1173987. doi: 10.3389/fnagi.2023.1173987. PMID: 37484689; PMCID: PMC10358778.
- Hagemann D, Meier JJ, Gallwitz B, Schmidt WE. Appetitregulation durch Ghrelin – ein neues neuroendokrines gastrales Peptidhormon der Gut-Brain-Achse [Appetite regulation by ghrelin – a novel neuro-endocrine gastric peptide hormone in the gut-brain-axis]. Z 2003 Sep;41(9):929-36. German. doi: 10.1055/s-2003-41853. PMID: 13130331.
- Furness JB. The Enteric Nervous System. Blackwell Publishing; 2006.
- Berthoud, H. R., and Neuhuber, W. L. (2019). Vagal mechanisms as neuromodulatory targets for the treatment of metabolic disease. N. Y. Acad. Sci. 1454, 42–55. doi: 10.1111/nyas.14182
- Matsubara Y, Kiyohara H, Teratani T, Mikami Y, Kanai T. Organ and brain crosstalk: The liver-brain axis in gastrointestinal, liver, and pancreatic diseases. 2022 Mar 1;205:108915. doi: 10.1016/j.neuropharm.2021.108915. Epub 2021 Dec 15. PMID: 34919906.
- Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, Scheimann J, Myers B. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response. Compr Physiol. 2016 Mar 15;6(2):603-21. doi: 10.1002/cphy.c150015. PMID: 27065163; PMCID: PMC4867107.
- Mayer, E. A., Savidge, T., and Shulman, R. J. (2014). Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology 146, 1500–1512. doi: 10.1053/j.gastro.2014.02.037
- Decarie-Spain L., Hayes A. M. R., Lauer L. T., Kanoski S. E. (2023). The gut-brain axis and cognitive control: a role for the vagus nerve. Cell Dev. Biol. 3, S1084-9521(23)00032–0. 10.1016/j.semcdb.2023.02.004 [PMC free article][PubMed] [CrossRef] [Google Scholar]
- Guo B, Zhang M, Hao W, Wang Y, Zhang T, Liu C. Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression. Transl Psychiatry. 2023 Jan 9;13(1):5. doi: 10.1038/s41398-022-02297-y. PMID: 36624089; PMCID: PMC9829236.
- Austelle CW, O’Leary GH, Thompson S, Gruber E, Kahn A, Manett AJ, Short B, Badran BW. A Comprehensive Review of Vagus Nerve Stimulation for Depression. 2022 Apr;25(3):309-315. doi: 10.1111/ner.13528. Epub 2021 Sep 6. PMID: 35396067; PMCID: PMC8898319.
- Ben-Menachem E, Hamberger A, Hedner T et al. Effects of vagus nerve stimulation on amino acids and other metabolites in the CSF of patients with partial seizures. Epilepsy Res 1995;20:221–227
- Giunta S, Xia S, Pelliccioni G, Olivieri F. Autonomic nervous system imbalance during aging contributes to impair endogenous anti-inflammaging strategies. 2023 Oct 11. doi: 10.1007/s11357-023-00947-7. Epub ahead of print. PMID: 37821752.
- Magnon V, Dutheil F, Vallet GT. Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep. 2021 Sep 29;11(1):19267. doi: 10.1038/s41598-021-98736-9. PMID: 34588511; PMCID: PMC8481564.
- Carabotti M., Scirocco A., Maselli M. A., Severi C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Gastroenterol. 28, 203–209. [PMC free article] [PubMed] [Google Scholar
- Blase K, Vermetten E, Lehrer P, Gevirtz R. Neurophysiological Approach by Self-Control of Your Stress-Related Autonomic Nervous System with Depression, Stress and Anxiety Patients. Int J Environ Res Public Health. 2021 Mar 24;18(7):3329. doi: 10.3390/ijerph18073329. PMID: 33804817; PMCID: PMC8036915
- Pham T, Lau ZJ, Chen SHA, Makowski D. Heart Rate Variability in Psychology: A Review of HRV Indices and an Analysis Tutorial. Sensors (Basel). 2021 Jun 9;21(12):3998. doi: 10.3390/s21123998. PMID: 34207927; PMCID: PMC8230044.
- Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018 Mar 13;9:44. doi: 10.3389/fpsyt.2018.00044. PMID: 29593576; PMCID: PMC5859128.
- C. Streeter, P.L. Gerbarg, R.B. Saper, D.A. Ciraulo, R.P. Brown. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Medical Hypotheses,Volume 78, Issue 5,2012,
- da Silva MA, Dorsher PT. Neuroanatomic and clinical correspondences: acupuncture and vagus nerve stimulation. J Altern Complement Med. 2014 Apr;20(4):233-40. doi: 10.1089/acm.2012.1022. Epub 2013 Dec 20. PMID: 24359451.
- Mikkelsen K, Stojanovska L, Polenakovic M, Bosevski M, Apostolopoulos V. Exercise and mental health. Maturitas. 2017 Dec;106:48-56. doi: 10.1016/j.maturitas.2017.09.003. Epub 2017 Sep 7. PMID: 29150166.