The Link Between Akkermansia Muciniphila and a Healthy Gut Barrier
Akkermansia muciniphila, a promising strain of bacterium discovered two decades ago, has gained an increase in recognition for its role in modulating a healthy gut barrier, which is crucial for countless aspects of our health. Not only is maintaining the integrity of the GI intestinal barrier imperative for digestion and absorption of nutrients, but also for brain function, metabolism, immunity, and regulating inflammation and oxidative stress in the body. This is significant, as inflammation is the leading driver of the majority of illnesses (1).
Lay of The Land – The GI Microbiome Ecosystem
Research pertaining to the vastness of the microbiome has boomed within the last two decades. The human microbiome has been suggested to comprise anywhere from 10 to 100 trillion microorganisms – a number that far exceeds that of human cells. In fact, the cells that make up the human body are more microbe than human, with 10% of cells regarded as human and 90% as microbe (2, 3).
The GI mucosa, or membrane layer, is the area where the interactions between our physiology and that of the external world occur. It is composed of four layers, each with specialized functions. The integrity of the intestinal barrier is significant for maintaining homeostasis, health, and overall protective function (4).
The gut microbiome is composed of a large ecosystem of microorganisms, including fungi, bacteria, and viruses (5). The genetic material of gut microbiota comprises more than 45 million genes (6). This highlights the promising role of the gut microbiome in modulating and influencing our health.
The gut microbiota and GI intestinal barrier communicate with each other via a complex network of physiological interactions. When these conditions are in balance, they contribute to improved markers of our health. This vast ecosystem is vital for immunity, energy metabolism and balance, and influences cognitive and mental health (7). Alterations in homeostasis can arise from diet, environmental and lifestyle factors, substances, and gut microbiota composition.
- muciniphila has emerged as a novel bacterium relative to the functioning of this integral ecosystem, as well as having a significant role in maintaining a healthy gut barrier or intestinal permeability. A. muciniphila is suggested to represent 3-5 % of the composition of the gut microbiota (8). Biochemical individuality, such as genetic variation, lifestyle, and environmental factors, account for differences in concentrations.
Slimy, Yet Integral – Akkermansia’s Role in Intestinal Permeability
The gastrointestinal barrier, or lining, separates our internal physiology from that of the external environment. It is coated by a thick layer of mucus, designed to absorb nutrients from the foods we consume into the bloodstream. Mucus contains mucins that are synthesized and released by goblet cells, with the integral function of protecting and lubricating the epithelium. Microbes, microbial toxins, and cytokines can affect mucin production, and thus compromise the mucus barrier, increasing susceptibility to insult and inflammation.
Akkermansia has protective and adaptive functions in the GI microbiome ecosystem, due to its role in maintaining intestinal mucus integrity. This is important as it prevents nutrients from leaking through and inducing stress in the system. When particles leak through the intestinal wall, they can contribute to inflammation and oxidative stress.
The integrity of the intestinal barrier is significant for digestion, absorption, and utilization of vital nutrients, as well as for metabolic health and energy balance (9). Compromised intestinal barrier permeability is linked with systemic inflammation, compromised digestion, and poor markers of metabolic health.
Increased intestinal permeability describes the flux of water-soluble compounds across the pathway of the small intestine. Intracellular enterocyte and tight junction proteins activated by Akkermanisa modulate the permeability of the membrane, as well as movement via this pathway. The intestinal barrier modulates the balance between tolerance, immunity, and inflammation. Altered intestinal permeability has been found to be associated with increased inflammatory cytokines, environmental toxins, and diet. Immune dysfunction can also lead to an increase in intestinal permeability and inflammation.
However, the factor that is most strongly associated with intestinal permeability is the diversity and composition of the gut microbiome. The composition of the gut microbiome, including diversity and quality of species can compromise or support the integrity of the intestinal barrier.
- muciniphila degrades mucins as energy sources to produce short-chain fatty acids (SCFAs), supporting metabolism and beneficial diversity of the GI microbiome (10).
Additionally, A. muciniphila strengthens the intestinal barrier by thickening mucus, thereby increasing integrity of the gut barrier lining. Through this mechanism, it also improves the ecosystem of the microbiome.
Metabolic Endotoxemia
A growing body of evidence in the field of Metagenomics, indicates that GI microbiota communities differ significantly in those with metabolic health conditions in comparison to those without (11). This is particularly noteworthy with regard to reduced concentrations of A. muciniphila. Research highlights a loss of abundance in this novel bacterium in those individuals with obesity and type 2 diabetes (12). The mechanisms that are suggested to be at play are improved intestinal permeability, increased diversity or dynamics of the gastrointestinal (GI) microbiome, and an overall decrease in systemic inflammation. These physiological mechanisms are affected by Akkermansia and other bacteria, having integral roles in intestinal permeability, metabolism, and systemic inflammation.
Metabolic endotoxemia refers to the increase in inflammatory molecules from these underlying mechanisms, resulting in a cascade of systemic inflammation, further impeding other aspects of health. A lack of diversity in the microbiome, altered intestinal permeability, and compromised metabolic and immune health have all been noted. Metabolic endotoxemia also references the manifestation of oxidative stress, secondary to inflammation and these factors.
Reduced concentrations or abundance of Akkermansia have been associated with an increase in low-grade inflammation. This is important as an emerging body of research suggests that the intestinal microbiome plays an integral role in regulating numerous conditions that all have inflammation as a driving, underlying factor. These implicated conditions include inflammatory bowel disease, obesity, type 2 diabetes, cardiovascular disease, and cancer. For instance, those with obesity have been shown to have metabolic endotoxemia – as the result of increased altered intestinal permeability and lack of diversity in the microbiome, leading to systemic inflammation and oxidative stress.
Diet and lifestyle play a crucial role in modulating the dynamics and composition of the gut microbiome ecosystem. Adequate nutrition, sleep, movement, and even mindful-based stress reduction can support microbial shifts that favor health. These changes are thought to be induced in as little as 24 hours. So, nutrition and lifestyle factors are truly foundational in improving metabolic, inflammatory, and immune health conditions (13).
Inflammatory Markers & Immune Health
Compromised intestinal permeability and composition of the GI microbiome can impede upon digestion, absorption, and utilization of nutrients. Alterations in these processes can also induce inflammation in the system and oxidative stress via leaky gut. Whereas modulating the integrity of the intestinal barrier with efficacious amounts of A. muciniphila and other beneficial bacteria can support immunity while limiting the onset of inflammation in the system (1).
The gut microbiome, relative to composition and diversity, has significant roles in modulating intestinal permeability and metabolic endotoxemia–induced inflammation (14). An innate immune response becomes induced when low-grade inflammation is recurring or chronic in the system due to an increase in circulating endotoxins, such as lipopolysaccharides (LPS). Alterations or compromised intestinal barrier permeability is closely related to the onset of metabolic and immune health conditions. This is the result of inflammation, altered intestinal permeability, and gut microbiome ecosystem imbalance. An increase in endotoxin concentrations is followed by elevated inflammatory markers such as interleukin-6 and interleukin-1-alpha, further impeding the system.
While the gut epithelial wall can be an efficient barrier that prevents absorption of such inflammatory molecules, modifications to the intestinal epithelial barrier allow molecules such as LPS to be absorbed and enter the bloodstream, resulting in the activation of further pro-inflammatory cytokines, and thus driving systemic inflammation. This is an example of how metabolic endotoxemia can result in several inflammatory conditions and significantly compromise immune health (13). On the contrary, a healthy, diverse ecosystem and strong gut lining can activate and strengthen the immune system (14).
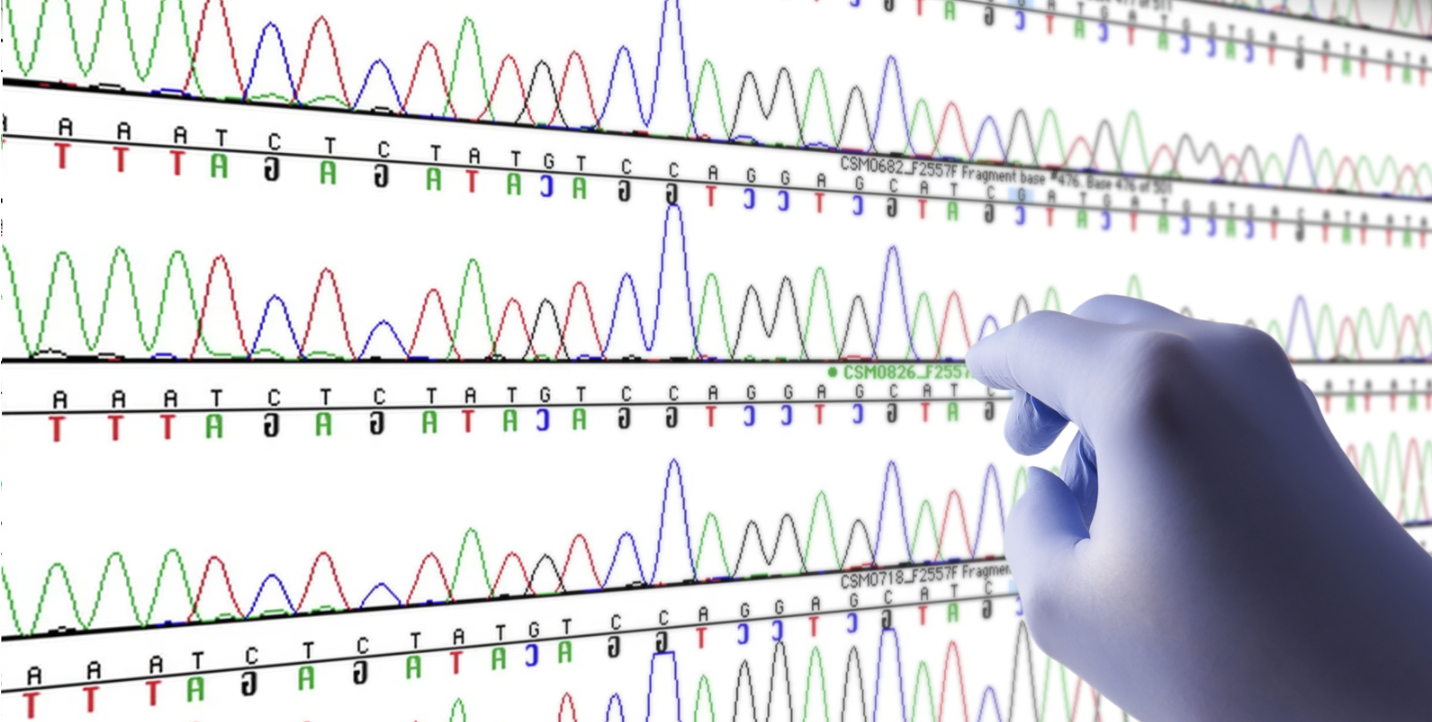
Microbial Differences & Implications
As emphasized, lower concentrations of Akkermansia have been found to impair the intestinal barrier, inducing changes to the gut lining, and the composition of gut microbiota. Since the discovery of this promising bacteria nearly 20 years ago, various studies have highlighted the lack of abundance of Akkermansia and its association with obesity, diabetes, inflammation, and cancer immunotherapies. Akkermansia’s main mechanisms of action include its intestinal symbiont properties – modulating inflammation and microbiome diversity and thereby influencing immune health. It is through this mechanism that the gut-immune system axis is supported.
Microbiome-Gut-Brain-Axis (MGB)
- muciniphila plays a comprehensive role in the microbiome-gut-brain axis through various mechanisms. This bacterium has protective functions relative to the intestinal mucosal barrier, and modulation of beneficial and diverse microbiota and metabolites, such as short-chain-fatty and amino acids, as well as the down-regulation of inflammation and harmful metabolites – all significant for maintaining homeostasis of the body’s physiological functions.
Akkermansia is suggested to have therapeutic implications through this axis in modulating mood health, as well as cognition. The following neurotransmitters have been evidenced to be synthesized in the gut: γ-aminobutyric acid (GABA), dopamine (DA), norepinephrine, and serotonin (5-HT) and thereby are affected by compromised function and composition (15).
Associations between depression, anxiety, and intestinal permeability have been well-cited in the literature. Akkermanisa is also suggested to have strong roles pertaining to neuropsychiatric disorders, including anxiety and depression, Alzheimer’s disease, cognitive impairments, substance use disorders, multiple sclerosis (MS), autism, epilepsy, Parkinson’s, stroke, and amyotrophic lateral sclerosis (ALS) (15, 16).
The underlying mechanisms suggested to be at play are inflammation, altered intestinal or gut barrier, and compromised GI microbiome balance, highlighting the potential therapeutic value of this novel bacterium (17).
The Plasticity of The Microbiome: Optimizing Abundance of Akkermansia
There are a number of strategies for improving and optimizing concentrations of this promising bacteria. Nutrition can enhance the abundance of Akkermansia in the GI tract, mucosa, and microbiome (18). Diet affects the mucus barrier via the microbiota, as it can increase the permeability of the mucus layer and mucus barrier dysfunction, increasing susceptibility to infection.
Increasing consumption of polyphenols can support the composition and rich diversity of the GI microbiome. Polyphenols found in green tea (such as catechin), grape seed (proanthocyanidins), and pomegranate (ellagic acid), have been shown to improve the environment of the ecosystem so that Akkermansia and other beneficial bacteria can thrive.
Prebiotics promote the abundance of beneficial bacteria and have also been found to support a healthy gastrointestinal tract and diverse intestinal microflora. Prebiotics are sources for beneficial strains of microbiota (such as Akkermansia) that support GI microbiome diversity while reducing intestinal and systemic inflammation. Sources of prebiotics include artichokes, bananas, chicory root, onions, and garlic. Increasing consumption of plant compounds, or phytonutrients, is also significant for modulating these aspects of health, as is ensuring nutrient density from anti-inflammatory fats and high-quality proteins.
As noted, a number of medications can contribute to altered intestinal permeability and compromised diversity in the intestinal microflora. Aspirin has been found to increase susceptibility to leaky gut, whereas antibiotics can greatly weaken the diversity of beneficial microbes (19).
In addition to nutrient density, obtaining sufficient sleep and regular movement are also significant for modulating microbiome health while supporting intestinal permeability.
It is also important to be mindful of stress, and other irritants to the integrity of the intestinal barrier and microbiome balance, including hallmarks of the Standard American Diet (SAD), such as refined carbohydrates, processed sugars, and overall inflammatory foods.
A Promising Bacteria to Improve Health
Novel strains of bacteria will continue to emerge with vast implications for improved health and well-being. The gut may be one of the most influential targets for intervention that we can modify and modulate, optimizing all aspects of health.
To learn more about the role this promising strain of bacterium has in intestinal permeability, and the collective ecosystem at large, view this webinar in which experts, Dr. Oubre, Dr. De Vos, and Dr. Bland discuss these profound and remarkable insights with implications for clinical practice.
References:
- Cani, P.D., Depommier, C., Derrien, M. et al. Akkermansia muciniphila: paradigm for next-generation beneficial microorganisms. Nat Rev Gastroenterol Hepatol 19, 625–637 (2022). https://doi.org/10.1038/s41575-022-00631-9
- Ursell LK, Metcalf JL, Parfrey LW, Knight R. Defining the human microbiome. Nutr Rev. 2012 Aug;70 Suppl 1(Suppl 1):S38-44. doi: 10.1111/j.1753-4887.2012.00493.x. PMID: 22861806; PMCID: PMC3426293.
- Cani PD, Osto M, Geurts L, Everard A. Involvement of gut microbiota in the development of low-grade inflammation and type 2 diabetes associated with obesity. Gut Microbes. 2012 Jul-Aug;3(4):279-88. doi: 10.4161/gmic.19625. Epub 2012 May 14. PMID: 22572877; PMCID: PMC3463487.
- Farhadi A., Banan A., Fields J., Keshavarzian A. Intestinal barrier: An interface between health and disease. Gastroenterol. Hepatol. 2003;18:479–497. doi: 10.1046/j.1440-1746.2003.03032.x.
- Vemuri R., Shankar E.M., Chieppa M., Eri R., Kavanagh K. Beyond Just Bacteria: Functional Biomes in the Gut Ecosystem Including Virome, Mycobiome, Archaeome and Helminths. 2020;8:483. doi: 10.3390/microorganisms8040483.
- Forster S.C., Browne H., Kumar N., Hunt M., Denise H., Mitchell A., Finn R., Lawley T.D. HPMCD: The database of human microbial communities from metagenomic datasets and microbial reference genomes. Nucleic Acids Res. 2016;44:D604–D609. doi: 10.1093/nar/gkv1216.
- Chelakkot C, Choi Y, Kim DK, Park HT, Ghim J, Kwon Y, Jeon J, Kim MS, Jee YK, Gho YS, Park HS, Kim YK, Ryu SH. Akkermansia muciniphila-derived extracellular vesicles influence gut permeability through the regulation of tight junctions. Exp Mol Med. 2018 Feb 23;50(2):e450. doi: 10.1038/emm.2017.282. PMID: 29472701; PMCID: PMC5903829.
- Belzer C, de Vos WM. Microbes inside—from diversity to function: the case of Akkermansia. ISME J 2012; 6: 1449–1458.
- Konig J, Wells J, Cani PD, Garcia-Rodenas CL, MacDonald T, Mercenier A et al. Human Intestinal Barrier Function in Health and Disease. Clin Transl Gastroenterol 2016; 7: e196.
- Karlsson CL, Onnerfalt J, Xu J, Molin G, Ahrne S, Thorngren-Jerneck K. The microbiota of the gut in preschool children with normal and excessive body weight. Obesity (Silver Spring) 2012; 20: 2257–2261
- Everard A, Belzer C, Geurts L, Ouwerkerk JP, Druart C, Bindels LB et al. Cross-talk between Akkermansia muciniphilaand intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci USA 2013; 110: 9066–9071
- Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, Abrouk M, Farahnik B, Nakamura M, Zhu TH, Bhutani T, Liao W. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017 Apr 8;15(1):73. doi: 10.1186/s12967-017-1175-y. PMID: 28388917; PMCID: PMC5385025.
- Zhang Y, Zhu X, Yu X, Novák P, Gui Q, Yin K. Enhancing intestinal barrier efficiency: A novel metabolic diseases therapy. Front Nutr. 2023 Mar 2;10:1120168. doi: 10.3389/fnut.2023.1120168. PMID: 36937361; PMCID: PMC10018175.
- Mohammad S, Thiemermann C. Role of Metabolic Endotoxemia in Systemic Inflammation and Potential Interventions. Front Immunol. 2021 Jan 11;11:594150. doi: 10.3389/fimmu.2020.594150. PMID: 33505393; PMCID: PMC7829348.
- Dicks LMT. Gut Bacteria and Neurotransmitters. Microorganisms. 2022 Sep 14;10(9):1838. doi: 10.3390/microorganisms10091838. PMID: 36144440; PMCID: PMC9504309.
- Ruiling Xu, Yuxuan Zhang, Shurui Chen, Yaohui Zeng, Xuan Fu, Ti Chen, Shilin Luo & Xiaojie Zhang(2023) The role of the probiotic Akkermansia muciniphila in brain functions: insights underpinning therapeutic potential, Critical Reviews in Microbiology, 49:2, 151-176, DOI: 1080/1040841X.2022.2044286
- Iordache MM, Tocia C, Aschie M, Dumitru A, Manea M, Cozaru GC, Petcu L, Vlad SE, Dumitru E, Chisoi A. Intestinal Permeability and Depression in Patients with Inflammatory Bowel Disease. J Clin Med. 2022 Aug 30;11(17):5121. doi: 10.3390/jcm11175121. PMID: 36079050; PMCID: PMC9457405
- Zhou K. Strategies to promote abundance of Akkermansia muciniphila, an emerging probiotics in the gut, evidence from dietary intervention studies. J Funct Foods. 2017 Jun;33:194-201. doi: 10.1016/j.jff.2017.03.045. Epub 2017 Mar 29. PMID: 30416539; PMCID: PMC6223323.of Akkermansia `
- Farhadi A, Gundlapalli S, Shaikh M. Susceptibility to gut leakiness: a possible mechanism for endotoxaemia in non alcoholic steatohepatitis. Liver Int. 2008